 Anthrax
Anthrax
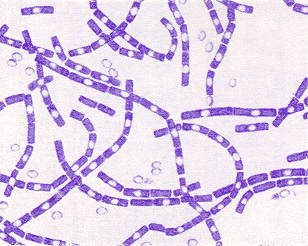
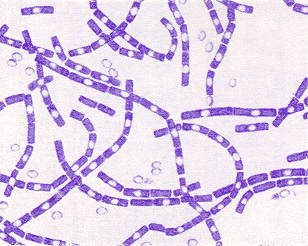
The bacterium Bacillus anthracis produces the three
components of anthrax toxin It is a gram positive spore forming rod, meaning
that it can survive for long periods of time in more extreme conditions
than non-spore forming bacteria. Furthermore, it can survive in aerobic
or anaerobic conditions. Spores of Bacillus a. can often be found
in the soil, even in geographical locations where anthrax is not a widespread
problem.
The incidence of anthrax in humans is quite
rare, although the awareness of anthrax as an agent of biological terrorism
has been boosted with the recent anthrax scare in the United States.
The most affected organisms are mammals but not humans; rather, the natural
occurrences of anthrax are in wild and domestic herbivorous animals such
as sheep, cattle, horses, mules, and goats.
Anthrax can be introduced into the affected
organism by three main routes. Cutaneous anthrax is an infection
resulting from the inoculation of an injured area or mucous membrane by
anthrax spores. Inhalation anthrax, the so-called “woolsorters disease”
is contracted by the inhalation of spores. The name is a reference
to the susceptibility of those who used to comb sheep wool to anthrax from
inhaling spore filled dust. Gastrointestinal anthrax begins in the
intestinal mucosa after ingestion of infected food (e.g. poorly cooked
meat). All of the conditions outlined above often prove fatal, especially
if only sub-standard treatment is available.
The anthrax toxin can more precisely be described
as “toxins” (plural) since there are 3 antigenic components: edema factor,
protective antigen, and lethal factor.
Lethal factor (LF)
 Anthrax
Anthrax