Coutesy of UCS: http://www.ucs.mun.ca/~cmtulk/index.html
Shigella dysenteriae cause a Bacillary dysentery disease.
The bacteria release the Shiga exotoxin that inhibits
protein sythesis by lysing 28S rRNA.
Coutesy of UCS: http://www.ucs.mun.ca/~cmtulk/index.html
Shigella dysenteriae cause a Bacillary dysentery disease.
The bacteria release the Shiga exotoxin that inhibits
protein sythesis by lysing 28S rRNA.
Shigella belong to the bacterial family, Enterobacteriaciae, and can occur as the four different species:
Shigella dysenteriae
Shigella flexneri
Shigella sonnei
Shigella boydii
They are gram-negative, citrate negative, H2S negative, lysine decarboxylase negative, non-lactose fermenting, bile salt resistant, facultative anaerobes that are non-motile and posses a capsule (K antigen) and an O antigen. These bacteria typically effect the higher primates, specifically, humans.
All four species produce a similar disease, shigellosis, which may vary in intensity, but elicits similar symptions in the host. Shigella are said to be the major cause of diarrheal disease and infant mortality throughout the developing nations of the world, and cause an estimated 15-20% of pediatric diarrhea in the United States. The species Shigella sonnei is the most comon cause of the disease, shigellosis in the United States and other developed countries, while Shigella flexneri is the most common cause of shigellosis in underdeveloped nations. However, the species that causes the most serious symptoms (including dysentery) is Shigella dysenteriae. This species occurs most frequently in the Eastern Hemisphere.
Only a small number of cells are required
for infection (200), thus shigella are spread easily via a fecal-oral
route, or even from direct person-to-person contact. Their generation
time is about 40 minutes, and the incubation period is only 1-7 days, averaging
3 days. Ingestion of contaminated food or water is also a mode of
infection, making proper sewage disposal and water treatment necessary
steps for prevention. Because of its association with crowded or
poor living conditions, this bacteria is often spread among people in prisons,
daycare centers, mental institutions, nursing homes, and military camps.
Daycare centers prove especially susceptable to shigellosis because of
the proportion of people under the age of 10yrs.
Secondary transmission
of the bacteria can occur, and the organism may be carried by its host
for an entire month after convalescence. Shigella can even be carried
by a host for several months by establishing a "chronic carrier condition,"
similar to other enteric bacterial infections.
Fig. 1: Mechanism of entry and dissemination of Shigella
in epithelial cells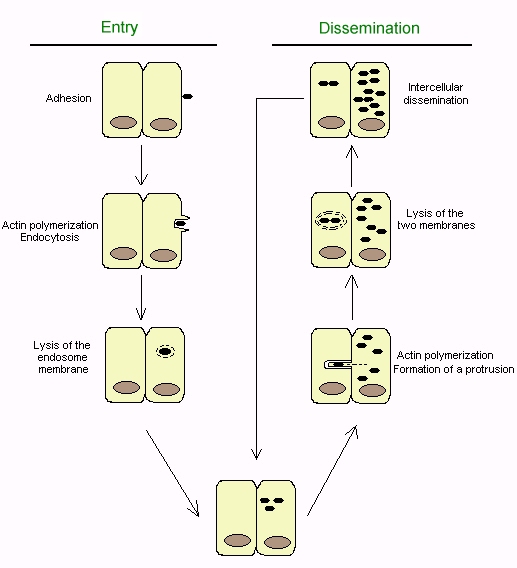
Shigella invade the villus cells of the large
intestine by penetrating the colonic mucosa, but do not invade the
blood, or perforate the intestine beyond the epithelium into the lamina
propria. Shigella enter the intestinal mucosa by attaching to,
and invading lymphoid cells in Peyer's patches. These
specialized lymphoid cells are called "M cells," and normally transport
foreign antigens from the intestine to underlying macrophages.
The bacteria are internalized by the epithelial cells via a process similar
to phagocytosis. This usually occurs with an endosome, but these
bacteria have the ability to lyse the phagocytic vacuoles of macrophage
cells and replicate in their cytoplasm (Fig 1.). The bacteria are
then spread into adjacent epithelial cells by propulsive movements of actin.
This way, the bacteria avoid antibody-mediated humoral immunity.
Shigella produce Ipa proteins in order to help escape
from the endosome, but also
From Parsot and Sansonetti (1996), Fig. 1, p.
27
produce them early on in order
http://www.ucs.mun.ca/~cmtulk/shigspread.htm
to initiate a cascade of cellular
signalization that internalizes the bacteria with endosomes.
While present in the mucosa, Shigella
typically cause an inflammatory response that results in extensive tissue
damage. They release a heat-stabile lipopolysaccharide endotoxin
that can cause fever. The LPS of Gram-negative bacteria contains
cell wall antigens (O antigens) that can elicit a variety of inflammatory
responses in an animal. This
endotoxin is part of the outer membrane of the Shigella cell, and has a
low degree of specificity and a low degree of potency. It has an
MW of 10kDa, and does not show enzymatic activity.
Shigella also use apoptosis in order to intentionally
activate the host's inflammatory response. Subsequent infiltration
and diapedisis by leukocytes disrupts the tight-junction of the bowel epithelium,
thus allowing a massive invasion by bacteria still in the colon, resulting
in a massive invasion and degradation of the intestinal mucosa.
From: http://www.surrey.ac.uk/SBS/ACADEMICS_homepage/mcfadden_johnjoe/SBS335.htm
Shiga Toxin Molecular Structure